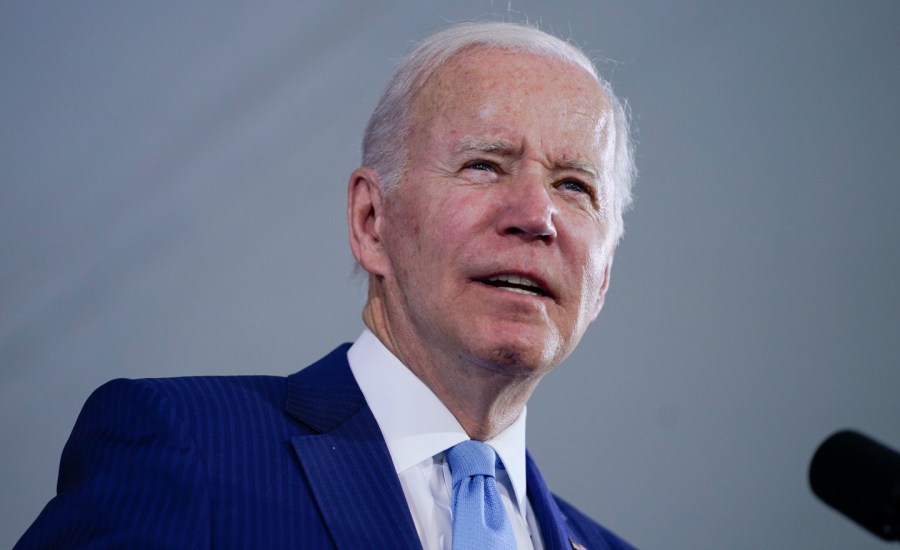
Health Care — Biden not immediately aware of baby formula crisis
In another example of how janitors aren’t paid enough, this custodian in California was able to trap a mountain lion that had gotten into a high school.
President Biden said he wasn’t aware of just how big an impact the shutdown of Abbott Nutrition’s infant formula plant and subsequent recall would have on formula availability.
Welcome to Overnight Health Care, where we’re following the latest moves on policy and news affecting your health. For The Hill, we’re Peter Sullivan, Nathaniel Weixel and Joseph Choi. Someone forward you this newsletter? Subscribe here.
Biden didn’t know extent of formula crisis until April
President Biden on Wednesday said he was not personally aware of the severity of the infant formula shortage until early April, months into the shutdown of a manufacturing plant operated by Abbott Nutrition and subsequent recall of its products.
“I became aware of this problem sometime in early April, about how intense it was. We did everything in our power from that point on,” Biden said during a White House roundtable with formula manufacturers.
“I don’t think anyone anticipated the impact of the shutdown of one facility,” Biden added.
Biden’s comments stand in contrast to administration officials, who have said repeatedly that the White House has been working around the clock since February to address the issue.
The president’s admission came minutes after executives from some of the leading manufacturers said they knew the shutdown would have a significant impact on formula availability.
When asked about the discrepancy, Biden noted: “They did, but I didn’t.”
The administration has been scrambling to respond to the formula shortage, which has frustrated parents across the country and seemed to catch officials by surprise.
Senators push for more mental health clinics
Sens. Roy Blunt (R-Mo.) and Debbie Stabenow (D-Mich.) are calling on lawmakers to expand Certified Community Behavioral Health Clinics (CCBHC) nationwide.
“This is an important moment to come together and finally treat health care above the neck the same as health care below the neck,” the senators wrote in a USA Today op-ed.
CCBHCs, which operate as nonprofit organizations or part of a local government, provide a range of mental health and substance use disorder services and are particularly aimed at helping vulnerable individuals.
Blunt and Stabenow helped establish an eight-state Medicaid demonstration program in 2014 to provide the centers with enhanced reimbursement rates to cover increased costs.
The centers are required to provide nine types of services to be designated as the special provider type in Medicaid, including 24-hour crisis care and integrations with physical health services.
“This approach is already changing people’s lives – and saving communities money – in the states where mental health and addiction treatment are funded the same way as other health care,” Blunt and Stabenow wrote.
FLORIDA HEALTH CARE PROVIDERS CHALLENGE 15-WEEK ABORTION BAN
A group of Florida health care providers filed a lawsuit Wednesday challenging the state’s new abortion law, which will go into effect next month.
The legislation, signed into law by Florida Gov. Ron DeSantis (R) in April, will go into effect on July 1.
The law will ban the procedure after 15 weeks of pregnancy and doesn’t include exemptions for rape, incest or human trafficking. However, the law does stipulate several exceptions, including cases in which a fatal abnormality is found or an abortion is needed to save the life or prevent serious injury to the pregnant person.
The lawsuit alleges that the bill — H.B. 5 — “radically curtails the ability of Floridians to make decisions about whether or not to continue a pregnancy and have a child,” which the petitioners say is in violation of their rights under the Florida Constitution.
American Civil Liberties Union (ACLU), ACLU of Florida, Center for Reproductive Rights, Planned Parenthood Federation of America, and the law firm Jenner & Block said they filed this lawsuit on behalf of a number of health care providers.
SMALL AMOUNTS OF SOME DRUGS DECRIMINALIZED IN BRITISH COLUMBIA
Small amounts of certain drugs like heroin, cocaine and meth will be decriminalized in British Columbia starting next year as the province grapples with rising opioid deaths.
Beginning Jan. 23, 2023, and going through Jan. 23, 2026, residents in British Columbia who have up to 2.5 grams of opioids, cocaine, methamphetamine or MDMA, also known as ecstasy, will not be arrested or face charges of possession of those drugs, according to the Canadian government.
The exemption is only applicable for British Columbia residents at least 18 years old. Possession of those drugs in certain areas, such as licensed child care facilities and airports, are not covered by the exemption.
Criminal charges are still applicable to those who carry higher amounts of the drugs.
The British Columbia government said in their own press release that police will offer assistance such as referrals for treatment for those who ask for it and provide additional information about social and health support resources.
Officials are hoping the policy change will direct more of those affected by the opioid crisis to get help. The province declared opioid addiction as a public health emergency in 2016.
Industry middlemen driving up prices of generic drugs
U.S. consumers are overpaying by billions of dollars for generic drugs due to the cost being driven up by middlemen in the pharmaceutical industry, according to a report from the University of Southern California (USC).
According to the white paper from USC’s Schaeffer Center for Health Policy and Economics, business practices carried out by pharmacy benefit managers (PBMs) have “inflated” the cost of generic medications.
The report cited the rise of generic medications as an American success story, as they allowed more people to access medicines and also enabled the U.S. health care system to save money. According to the most recent estimates cited by USC, generic medications are dispensed 97 percent of the time when they are available.
However, as insurance companies began covering more medicines, sellers began raising the prices, as most consumers did not know the actual cost of their prescriptions, only what they paid at the counter, the report said.
The role that PBMs play in the rising cost of medications has been noted for some time. One way in which PBMs profit off of prescriptions is through a practice called “spread pricing,” which is when they reimburse a pharmacy for one price while also charging health insurance providers a higher price and keeping the difference, or the “spread.”
“Commercial tactics such as spread pricing, copay clawbacks and formularies that advantage branded drugs over less expensive generics have funneled the savings from low-cost generics into intermediaries’ pockets, rather than the pockets of patients,” the report said.
WHAT WE’RE READING
- Costly Alzheimer’s treatment is spreading around the world, with virtually no science to back it up (Stat)
- Wray: FBI blocked planned cyberattack on children’s hospital (Associated Press)
- Vaccine injury compensation programs overwhelmed as congressional reform languishes (Politico)
STATE BY STATE
- Justice Department says sweeping lab test fraud in Texas involved dozens of doctors and front companies (Stat)
- ‘Desperate situation’: states are housing high-needs foster kids in offices and hotels (Kaiser Health News)
- Tribal leaders sound the alarm after fentanyl overdoses spike at Blackfeet Nation (NPR)
That’s it for today, thanks for reading. Check out The Hill’s Health Care page for the latest news and coverage. See you tomorrow.
Copyright 2024 Nexstar Media Inc. All rights reserved. This material may not be published, broadcast, rewritten, or redistributed..











